Introduction: Why Clinical Trials Matter
Clinical trials fuel the advancement of medical knowledge. They allow researchers to test how well a new drug, procedure, or treatment approach works, while also identifying side effects. In clinical trials, volunteers are the real heroes. By participating, they contribute to valuable findings that may benefit thousands—or even millions—of patients in the future.
Many of the medicines and treatments we use today exist because volunteers took part in a clinical trial at some point. Through these trials, doctors learn about effectiveness, safety, and long-term impacts on patients. In other words, when we talk about clinical trial steps, we are describing the process that leads to safer and more effective therapies around the globe.
Clinical trials follow strict guidelines, regulated by government agencies like the Food and Drug Administration (FDA) in the United States and similar organizations worldwide. These rules protect participants' rights and safety. This section explains how clinical trials are organized and why they function in specific phases.
The Definition of a Clinical Trial
A clinical trial is a research study performed in people that aims to test whether a medical strategy, treatment, or device is safe and effective. Trials can explore vaccines, new medicines, surgical methods, or innovative uses of existing treatments. Each clinical trial must meet precise scientific and ethical standards to keep patients safe and produce reliable results.
Who Oversees Clinical Trials?
Regulatory bodies, independent ethics committees, and Institutional Review Boards (IRBs) closely monitor clinical trials to ensure participant welfare. They evaluate the trial plan (protocol) before it starts and continue to oversee the trial to ensure it follows the approved guidelines for safety and ethics. This system helps maintain public trust and uphold the highest standards.
Clinical trials usually progress through four main phases, each with specific goals and types of questions.
| PHASE | GOAL | NUMBER OF PARTICIPANTS |
|---|---|---|
| I | Safety and proper dosage | Small group (20–80 participants) |
| II | Efficacy and short-term side effects | Larger group (100–300 participants) |
| III | Comparison with current treatments and safety data | Even larger group (1,000+ participants) |
| IV | Post-approval research and long-term effects | Varies (often thousands of people) |
Phase I:
Researchers test the new treatment in a small group to determine the safest dosage and identify serious side effects. Safety is the main focus.
Phase II:
The treatment’s effectiveness is tested with a larger group. Researchers continue to monitor for side effects and adjust dosages if necessary.
Phase III:
The treatment is tested against the current standard of care in a much larger, often global, group. This phase gathers enough information for regulatory approval.
Phase IV:
After approval, researchers monitor the treatment’s long-term effectiveness and any rare or long-term side effects in a larger population.
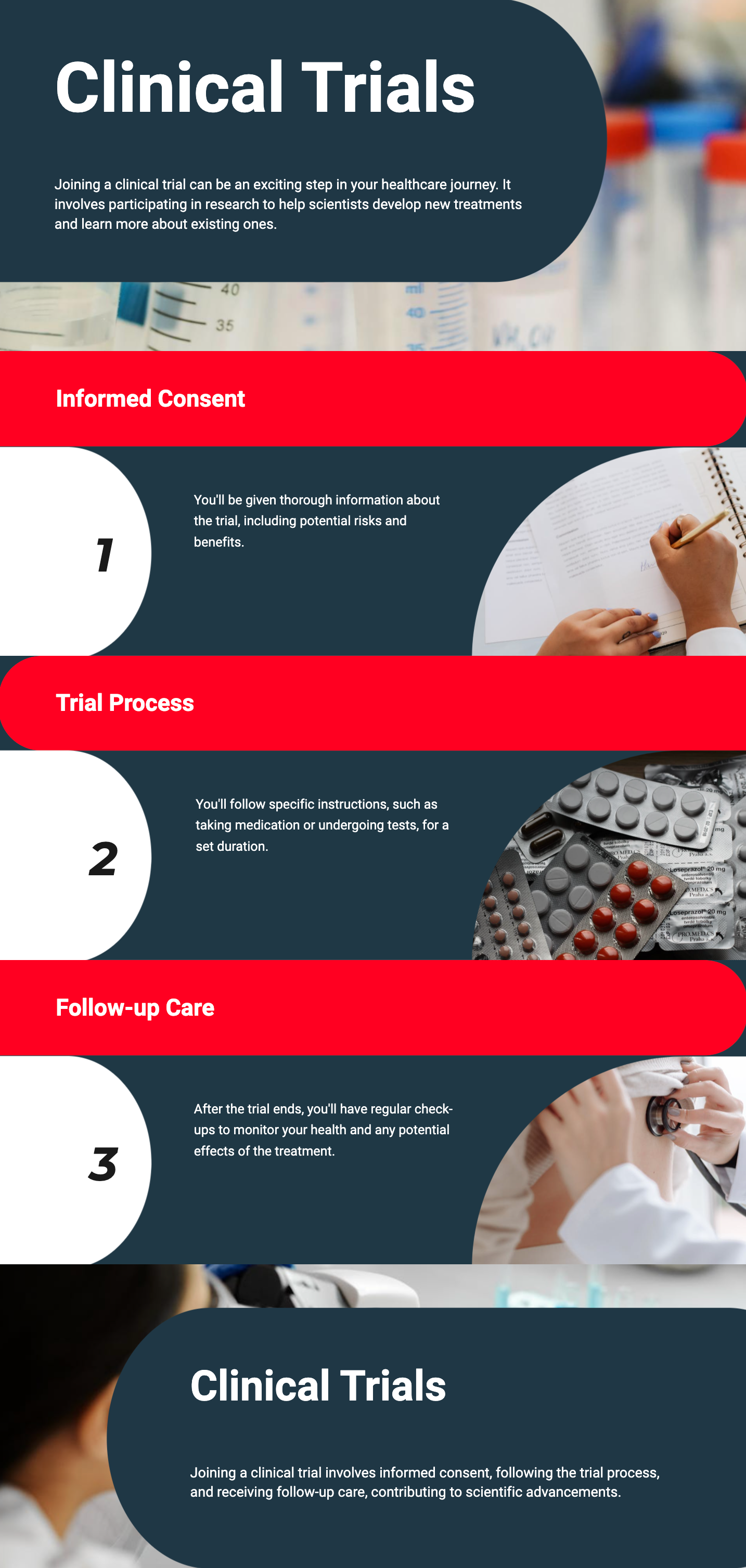
If you are considering joining a clinical trial, understanding the enrollment process is crucial. Researchers will review your medical history, discuss the trial requirements, and determine if you meet eligibility standards.
The Enrollment Process
The research team shares detailed information about the clinical trial, including its purpose, duration, required tests, and potential side effects. They will also discuss any costs or reimbursements. Some clinical trials offer compensation for travel or time spent; others may not.
Before you agree to participate, you’ll have time to ask questions. The team will explain how your data will be collected and protected.
Your Rights and Informed Consent
Informed consent ensures you understand all aspects of the clinical trial. You’ll receive a document that outlines key information, and you’ll have the opportunity to ask important questions, such as:
Signing the informed consent form means you voluntarily agree to participate, but you can withdraw at any time.
Screening and Pre-Assessment
After signing the consent form, you undergo a screening phase. Here, the team assesses your health status to ensure you meet the clinical trial’s specific inclusion criteria. They may also perform tests like blood work or imaging scans. This ensures participant safety and the collection of consistent, high-quality data.
Once enrolled, you’ll follow a specific schedule that may involve doctor visits, lab tests, medications, and check-ins. The exact commitment depends on the trial design.
Monitoring and Ongoing Care
Medical professionals monitor you throughout the clinical trial. They track vital signs, symptoms, and any side effects. If problems arise, they may adjust the treatment or recommend you stop participating for safety reasons.
Communication is key — you're encouraged to report any changes in your health.
Potential Side Effects
Side effects are a possibility in any clinical trial. Reporting unusual symptoms early allows researchers to intervene quickly, whether by adjusting doses or providing additional treatments.
The Role of Placebos
Some clinical trials use placebos (inactive treatments) or compare the new treatment to the standard of care. Participants may not know which group they are in (blinding) to prevent bias. Placebos are only used when ethically appropriate — when no proven effective therapy exists.
Before joining, weigh the potential benefits and risks:
Potential Benefits:
Potential Risks:
Speak with your doctor, the research team, and loved ones to make the best decision for you.
When the clinical trial concludes, you might be asked for follow-up visits or feedback. Final exams or tests may also be required. Some participants continue using the treatment if it was effective and safe, depending on trial policies.
Remember: Even if results aren't immediately visible in mainstream care, your participation advances future treatments.

Joining a clinical trial is a significant decision that blends hope, curiosity, and dedication to advancing medicine. From initial enrollment to follow-up, every step is designed with patient safety in mind. Although challenges like side effects or additional appointments may arise, the opportunity to contribute to life-changing treatments makes clinical trials a powerful path to consider. Always consult your healthcare providers and loved ones before making a final decision.
Yes. You can withdraw at any time, and it won’t affect your future healthcare.
Often no. Many trials cover costs and may offer travel or lodging reimbursements. Confirm details with the research team.
Strict privacy regulations ensure your data is coded or anonymized. Only essential personnel can access identifying information.
Your safety comes first. The research team will provide immediate care, adjust treatment if needed, or remove you from the clinical trial for safety.
Yes. It’s important to keep your primary physician involved in your care during the trial.
 05.03.2025
05.03.2025