Telemedicine has reshaped the way healthcare is delivered, offering accessibility and convenience like never before. In the wake of the COVID-19 pandemic, its adoption surged as healthcare providers sought innovative solutions to continue patient care remotely. But what does the future of telemedicine hold? Will it continue to thrive or fade away as in-person visits return? In this article, we explore how telemedicine is evolving, the challenges it faces, and the ways it is bridging healthcare gaps in a post-pandemic world.
Telemedicine has been around for decades, but it wasn’t until the pandemic that its potential was fully realized. Patients who once hesitated to see a doctor virtually became comfortable with remote consultations. Hospitals and clinics, too, embraced digital health tools to minimize risks and streamline care.
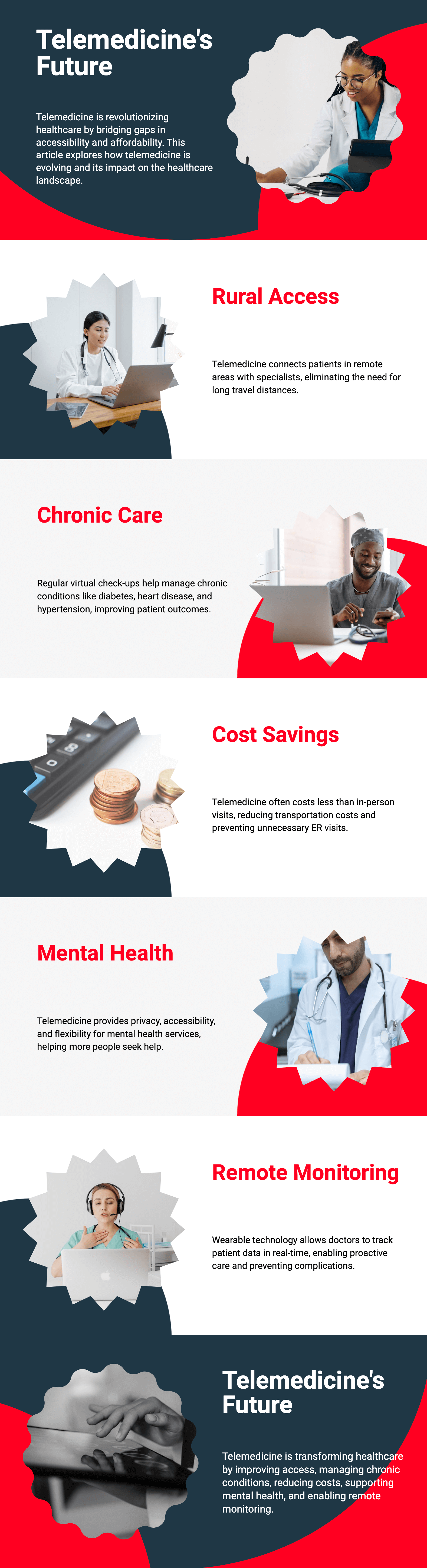
Key Drivers of Telemedicine Growth:

1. Expanding Access to Rural and Underserved Areas
Millions of people in rural areas lack access to quality healthcare due to provider shortages. Telemedicine eliminates distance barriers, allowing patients to consult specialists without traveling long distances.
2. Enhancing Chronic Disease Management
Patients with chronic conditions like diabetes, heart disease, and hypertension require regular check-ups. Telemedicine enables frequent monitoring, reducing hospital visits while improving disease management.
3. Reducing Healthcare Costs
Virtual consultations are often cheaper than in-person visits. By cutting transportation costs and preventing unnecessary ER visits, telemedicine can significantly lower healthcare expenses.
4. Mental Health Support
Mental health services have seen a major boost through telemedicine. Virtual therapy sessions provide privacy, accessibility, and flexibility, making it easier for patients to seek help.
5. Remote Patient Monitoring (RPM)
Wearable technology and smart devices now allow doctors to track patients’ health data in real time. This proactive approach prevents complications and ensures timely interventions.
Despite its rapid adoption, telemedicine is not without challenges.
1. Digital Divide and Internet Connectivity Issues
Many low-income populations lack access to high-speed internet, limiting their ability to use telemedicine effectively. Addressing this digital gap is essential for equitable healthcare.
2. Regulatory and Insurance Barriers
Telemedicine laws and reimbursement policies vary widely across regions. Standardized regulations will be crucial for long-term telehealth success.
3. Security and Privacy Concerns
As more patient data moves online, cybersecurity risks increase. Strong encryption and data protection measures are needed to maintain patient trust.
4. Limited Physical Examination Capabilities
Certain conditions require in-person evaluations, limiting telemedicine’s effectiveness for some diagnoses and treatments. Hybrid models combining virtual and physical visits may be the solution.
Artificial intelligence (AI) and machine learning are transforming telemedicine in profound ways.
1. AI-Powered Diagnostics
AI can analyze medical images, detect diseases early, and assist doctors in diagnosing conditions faster and more accurately.
2. Chatbots and Virtual Health Assistants
AI-driven chatbots can provide 24/7 medical advice, schedule appointments, and answer patient questions, reducing the burden on healthcare staff.
3. Blockchain for Secure Health Data Sharing
Blockchain technology enhances security and interoperability, allowing patients to safely share their medical history across different healthcare providers.
4. Virtual Reality (VR) and Augmented Reality (AR) in Telemedicine
VR and AR are being explored for remote surgery training, rehabilitation programs, and even virtual patient interactions.
Telemedicine is no longer just a temporary fix—it is a permanent part of modern healthcare. Here’s what we can expect in the coming years:
1. Hybrid Healthcare Models
The future will likely see a combination of in-person and virtual visits, optimizing care delivery for both convenience and effectiveness.
2. Increased Insurance Coverage for Telehealth
As telemedicine proves its value, more insurance companies are expected to expand coverage, making virtual care more accessible.
3. Improved Telemedicine Infrastructure
Governments and the private sectors will invest in better digital health infrastructure, ensuring broader access to telemedicine services.
4. Personalized and AI-Driven Healthcare
AI will make telemedicine more tailored to individual patient needs, offering predictive analytics and personalized treatment plans.
5. Expansion into Global Health
Telemedicine has the potential to provide medical expertise across borders, improving healthcare access in developing countries.
Telemedicine has proven to be a game-changer, transforming the way healthcare is delivered. While challenges remain, advancements in technology, regulatory support, and growing patient acceptance indicate that telemedicine is here to stay. By addressing current limitations and enhancing accessibility, telemedicine will continue to bridge healthcare gaps, making quality healthcare available to all, regardless of location or socioeconomic status.
No, telemedicine complements in-person visits rather than replacing them. A hybrid approach that integrates both virtual and physical consultations is expected to be the future of healthcare.
Coverage varies depending on the country and insurance provider. However, many insurers are expanding their telehealth policies due to its growing demand and proven effectiveness.
Telemedicine platforms use encryption and data protection measures to ensure patient privacy. However, choosing HIPAA-compliant and secure telehealth services is recommended.
Typically, a smartphone, tablet, or computer with a stable internet connection and a webcam is sufficient. Some consultations may require additional medical devices like blood pressure monitors or wearable health trackers.
Telemedicine allows quick consultations, triaging patients remotely, and providing immediate medical advice, which can be life-saving in emergencies.
 28.02.2025
28.02.2025